Table of Contents
Introduction: Transformative Shifts in Healthcare
Globally, several emerging macro trends are pushing the healthcare industry to evolve. These trends are driven by changes in demographics, technological advancements and an increased focus on tailored, patient-centered care.
While it is impossible to predict the future with certainty, certain macro trends are likely to significantly impact the healthcare industry in coming years. These transformative shifts are poised to reshape the way healthcare is delivered and received, with implications for patients, healthcare providers and policymakers.
The Aging Population
Clearly one of the most significant trends affecting the healthcare industry is the aging population. As baby boomers age, there is an increased demand for healthcare services. This has led to a surge in chronic noncommunicable diseases such as diabetes, cardiovascular disease and Alzheimer’s. Healthcare providers must adapt to the needs of an aging population by developing new models of care and investing in innovative technologies that improve patient outcomes while reducing the cost of care.
Technological Advancements
Technology continues to revolutionize the healthcare industry. From telemedicine to electronic health records, it’s easier than ever for healthcare providers to deliver care to patients with improved speed and quality. Wearable devices and mobile health applications have also become more prevalent, allowing patients to monitor their health and receive real-time feedback. Advances in artificial intelligence and machine learning have the potential to significantly impact the way healthcare is delivered by providing personalized treatments and predicting patient outcomes.
Precision Medicine
The precision medicine trend, also called personalized medicine, tailors treatments to individual patients based on their needs and genetic makeup. This approach has tremendous potential to improve patient outcomes and reduce healthcare costs. Through pharmacogenomic analysis, healthcare providers can make more informed decisions about which treatments and medications are most likely to be effective. This reduces the likelihood of negative reactions to medications and unnecessary treatments – ultimately saving the consumer money and leading to better health outcomes. Precision medicine has the potential to revolutionize healthcare delivery, benefiting patients and healthcare providers. As a result, this trend has led to increased investment in genomic research and the development of targeted therapies.
Healthcare Consumerism
Patients are becoming more informed and involved in their healthcare decisions, leading to the rise of consumerism in healthcare. Patients are demanding more transparency in pricing, easy access to their medical records and greater convenience when accessing healthcare services. This trend is driving healthcare providers to focus on delivering patient-centric care that prioritizes the patient experience.
Healthcare Policy
Healthcare policy changes significantly influence the healthcare industry. Changes in government healthcare initiatives and healthcare legislation can have a profound effect on the way healthcare is paid for and delivered. The Affordable Care Act (ACA) is one example of a policy that has increased access to healthcare services for millions of Americans. As healthcare policy continues to evolve, healthcare providers need to be prepared to adapt to changes in reimbursement models and regulations.
Living Longer, Living Better: The Implications of Increasing Life Expectancy
Globally, the population is living longer than ever on average, biasing the global average population age toward the more elderly. This trend is also driven by declining fertility rates, improved medical care and advancements in public health – and its effect is being felt worldwide.
According to the United Nations, the number of people aged 60 and above is expected to double by 2050 and triple by 2100. By 2050, projections suggest there will be 2.1 billion people over the age of 60, accounting for 21% of the global population. Figure 1 demonstrates the demographic shifts that coincide with population distribution as a function of age. The more rounded a plot is, the more its given region is aging. If the population is contracting, the plot starts to recede.


The aging population has implications for healthcare systems worldwide. As people age, they are more likely to develop chronic noncommunicable diseases (e.g. cancer, cardiovascular disease, etc.). These conditions require ongoing medical care and support, which can strain healthcare resources. The aging population also places a greater demand on long-term care services such as nursing homes and home healthcare.
The economic impact of this aging population is also significant. Older individuals tend to have lower participation rates in the workforce, which can lead to a decline in economic productivity. Additionally, as the number of older individuals increases so does the demand for social security and pension programs, affecting government budgets and regional economies.
These developments have enabled older individuals to maintain their independence, stay active and engaged in their communities, and enjoy a better quality of life in their later years. Additionally, new technologies and innovations in healthcare have made it easier for older people to manage chronic conditions and maintain their overall health and well-being, allowing them to enjoy more active and fulfilling lives as they age. While there is still more work to be done to ensure that all older individuals have access to the resources and support they need to maintain their quality of life, there is no doubt that progress has been made in this area.
To address these challenges, healthcare systems need to adapt to older individuals’ changing needs. This includes investing in preventative care, developing new models of care that focus on patient centered approaches and using technology to improve healthcare delivery. Governments also need to implement policies that support older individuals, expand access to social services and develop programs that promote healthy aging.
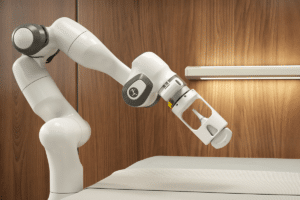
Robotics and automation are also emerging as promising solutions to the economic challenges that come with an aging population. With fewer working-age individuals to support older adults, robotics and automation can help fill critical labor shortages, improving productivity and efficiency in a range of industries. For example, robots and automation can be used to perform routine tasks, such as automated drug dispensing and delivery. This frees up healthcare providers to focus on more complex and specialized care. Additionally, robots and automation can improve manufacturing processes, leading to higher output and increased competitiveness for businesses. By reducing the burden on the workforce and increasing efficiency, robotics and automation can help support economic growth and stability in the face of an aging population.
Transformative Health-Tech
Technological advancements have been key in improving patient outcomes over time. For instance, prior to the discovery of penicillin the most basic infection could have been life-threatening. Since the start of the COVID-19 pandemic, there have been several advancements transforming the way healthcare is being delivered, managed and experienced. Initially this was out of necessity, but several of these advancements or trends have persevered.
Telehealth or Telemedicine
COVID drove the use of technology to deliver healthcare services remotely via video conferencing, remote monitoring and mobile health apps. This expanded access to care, particularly for individuals living in rural or remote areas, and made it easier for patients to manage chronic conditions from the comfort of their own homes. By removing geographic limits, these services are making it easier than ever for individuals to find ideal healthcare providers – especially in more rural regions.
Electronic Health Records (EHRs)
The increased need for telehealth services has also driven the need for digital patient records that allow medical histories, treatments and test results to be accessed and shared securely by (or between) healthcare providers. EHRs improve the efficiency and accuracy of medical records, reducing errors and enabling providers to make more informed decisions about patient care.
While this might not sound like a major area for technological advancement, one recent study found that data generated from healthcare is set to reach a CAGR of 36% and currently represents approximately 30% of all data stored. Managing this data and the speed of its access (especially between providers) will continue to be a challenge for the foreseeable future.
Artificial Intelligence (AI)
The use of computer algorithms and machine learning to analyze and interpret vast amounts of medical data, such as medical images or patient records, is on the rise. AI has the potential to improve diagnostic accuracy, personalize treatments and support clinical decision-making.
Chat GPT in particular has the ability to interpret medical results by using natural language processing (NLP) algorithms and machine learning techniques. Chat GPT can analyze large volumes of medical data such as EHRs, medical images and laboratory results, then extract meaningful insights and patterns – all tasks that might overwhelm a healthcare provider. With limited time to review patient histories and the ever-growing amount of patient data collected, AI has the potential to improve the speed and accuracy with which diagnoses can be performed.
The internet has shown several examples of how Chat GPT can interpret laboratory results, such as blood tests or genetic tests. Chat GPT analyzes these results and identifies patterns that may indicate the presence of medical conditions or genetic predispositions that a healthcare provider may not see. Other real world examples of how AI has been leveraged come from Google Health. Researchers developed a deep learning model to predict kidney injury days in advance of traditional methods. Previously, this was typically only discoverable after the injury occurred. This evidence shows how AI may be able to outperform humans when predicting the onset of severe medical conditions.
Despite the potential benefits, there are still many risks to consider. AI systems can produce errors, and in healthcare those errors could cause patient injury or other problems. False negatives and false positives can have detrimental effects on a patient. The wrong drug recommendation or failure to detect a tumor can cause real harm. It’s fair to argue that human-generated errors already occur in the healthcare system; however, AI errors are potentially different in that patients and providers may react differently to software-based errors out of a tendency to trust information coming from a ‘machine’. Additionally, errors in widespread AI systems could potentially harm a larger number of patients than an individual provider’s mistake.
At their core, these AI models rely on data. If particular attention isn’t paid to the distribution of this data, there is strong potential for bias in the results – which may also negatively impact those who aren’t represented in the training data sets based upon any number of metrics (age, sex, race, etc.). Even though there is more healthcare data available today than ever before, researchers developing these models typically use small data sets. For good reason, there are many barriers to sharing patient data broadly, meaning that developers don’t have access to all (or even most) patient data. When they can access data, they may not even know about its inherent upstream bias.
Prematurely releasing AI products to the market or not properly evaluating their risks may lead to widespread flaws in medical diagnoses. For these reasons and more, the U.S. Food and Drug Administration (FDA), Health Canada and the United Kingdom’s Medicines and Healthcare products Regulatory Agency (MHRA) have jointly identified guiding principles that can inform the development of Good Machine Learning Practice (GMLP).
Wearable and Implantable Devices
Devices can be worn or implanted to monitor various health parameters such as heart rate, blood glucose levels or medication. These devices can provide patients and healthcare providers with real-time data on health status, enabling earlier interventions and more personalized care.
Insurance companies are encouraging the use of wearable devices in a number of ways. One approach is by offering discounts or incentives to policyholders who use wearable devices to track their health and fitness. For example, some insurance companies offer discounts on premiums or cash rewards to customers who use wearable devices to track their steps, monitor their heart rate, or manage chronic conditions like diabetes or hypertension. Additionally, insurance companies are using wearable device data to develop personalized health and wellness programs for their policyholders. By analyzing data from wearable devices, insurers can identify patterns and trends in their customers’ health and behavior and use this information to develop targeted interventions and wellness programs. For example, insurers might use wearable device data to identify customers at risk for developing chronic conditions like obesity or diabetes, then offer personalized coaching and support to help them manage their health more effectively.
Precision Medicine
Precision – or personalized – medicine is an approach to healthcare that tailors medical treatment to the individual patient. It considers a patient’s genetics, environment, lifestyle and medical history, then uses those factors to inform targeted, individualized treatment plans that are more effective and less likely to cause side effects.
Precision medicine is changing the way healthcare is delivered. With the availability of genetic testing and other personalized diagnostic tools, healthcare providers are able to identify patients who are at higher risk for certain diseases or conditions and develop targeted prevention and screening strategies. This can lead to earlier diagnosis and treatment, improving patient outcomes and reducing healthcare costs. Additionally, advancements in automation and imaging technologies have allowed for the creation of cost-effective, tailored medical devices. These tailored devices include items such as custom foot orthotics, clear aligners for teeth and customized implant devices used in arthroscopic surgeries.
Of all the medical technology innovations impacting precision medicine, technologies involving genetic sequencing may have the greatest overall impact. With recent advances in genetic sequencing technology, it is now possible to sequence a person’s entire genome in a matter of days or weeks. In addition to improved speed of sequencing, the cost of sequencing has also fallen dramatically. The National Human Genome Research Institute (NHGRI) has reported that the cost of sequencing is actually falling faster than what Moore’s Law would predict when normalizing the data against the semiconductor market as a comparative benchmark. The falling cost and increase in sequencing throughput has opened up new opportunities for personalized medicine, as access to this genetic information is now generally accessible and can be used to tailor medical treatment to an individual’s specific genetic makeup.
As a result, personalized medicine is making a difference in treating chronic or serious ailments. Perhaps the most significant impact has been seen in cancer treatments. By sequencing a patient’s tumor, doctors can identify specific genetic mutations that are driving the growth of the cancer. This information can be used to develop targeted therapies that block the mutations’ activity, improving treatment efficacy and reducing side effects.
Genetic sequencing has also been instrumental in identifying patients who are at higher risk for certain diseases or conditions. By analyzing a person’s genetic makeup, doctors can identify genetic markers that are associated with an increased risk of developing certain diseases or conditions. This information can be used to develop targeted prevention and screening strategies, allowing doctors to identify and treat these conditions earlier. For example, it is common practice to test developing fetuses for genetic conditions or chromosomal abnormalities while still in the womb, in an effort to identify conditions that might predict complications or require intervention.
In addition, genetic data is being used to identify patients who are likely to respond poorly to certain medications or combinations of medications. Pharmacogenetics is the study of how an individual’s genetic makeup influences their response to drugs. This type of personalized medicine optimizes drug therapy by tailoring treatment to an individual’s genetic profile. This information can be used to develop targeted treatment plans that are more effective and less likely to cause side effects. Pharmacogenetic testing is not yet routinely performed for all drugs and conditions, and more research is needed to fully understand the complex interactions between genetics and drug response. As the cost of testing continues to fall and opportunities for improving patient outcomes persist, this will be a key area of investigation for the foreseeable future.
In addition to the advances delivered by genetic sequencing technology, customized medical devices are now becoming commonplace in households worldwide. These devices, which range from simple prosthetics to more complex implantable devices, are designed and manufactured specifically for an individual patient. Historically, medical device OEMs relied on common sizes of mass-produced devices. However, patients often have anatomic and/or medical needs that render the available device sizes or shapes unsuitable.
Computer-aided surgery has helped in this domain, leveraging software to model how to fit standard devices as appropriately as possible; however, this approach may remove more tissue than needed to achieve the right fit. With advancements in imaging technology and automation, it is now possible to produce customized devices. 3D-printing has enabled the production of highly customized medical devices, such as hearing aids, dental implants and surgical instruments. These devices can be designed and manufactured to fit a patient’s exact specifications, improving their efficacy and comfort.
Advances in automation technologies have been key to making these personalized devices, or therapies, accessible. Automation significantly enhanced genetic sequencing, making it faster, more efficient and more cost effective. Previously, genetic sequencing was a time consuming, expensive process requiring specialized equipment and highly trained technicians. However, with the advent of automation technology, genetic sequencing has become much more accessible to researchers and healthcare providers. This has greatly accelerated the pace of genetic research and made it possible to quickly identify genetic mutations and markers associated with diseases and other health conditions. Similarly, automation is key to the production of customized medical devices. Given the speed, flexibility and precision available, it is now possible to produce cost-effective tailored medical devices at scale.
Empowered Patients
The shift towards patient-centered care emphasizes the role of patients as active consumers of their healthcare information, which is often accessed via apps and other digital healthcare solutions. This approach aims to empower patients to take greater control over their health and healthcare decisions by providing them with more information, greater access to healthcare services and a more personalized healthcare experience. Patients are becoming more engaged in their healthcare decisions, seeking out information on treatments and outcomes and demanding greater transparency and accountability from healthcare providers.
As a result of this shift towards consumerism, healthcare providers are adapting their practices to meet patient demands for greater convenience, accessibility and affordability. This is evident in the increasing availability of telehealth services and online access to medical records and test results.
Consumerism in healthcare is also driving healthcare technology innovation, with the development of wearable devices, mobile health apps and other tools that empower patients to monitor their health and manage chronic conditions more effectively.
While the rise of consumerism in healthcare has the potential to improve patient outcomes and increase patient satisfaction, it also presents challenges for healthcare providers and policymakers. Ensuring that patients have access to high-quality, evidence-based healthcare information and services while also controlling costs and maintaining the overall quality of care is an ongoing challenge that requires collaboration and innovation across the healthcare system.
Furthermore, there is concern that patients could become too dependent on seemingly automated results delivered digitally. Without oversight from healthcare professionals, there is significant potential for errors that may lead to misdiagnosis.
Trends in Healthcare Policy
With the mass of data now available, the policy environment is quickly adapting. Data is now a means of measuring provider performance. This is the foundation for an emergent healthcare policy trend called value-based care. Value-based care aims to improve patient outcomes while reducing healthcare costs. In a value-based care model, healthcare providers are incentivized to deliver high-quality care that meets the needs of individual patients, rather than performing more procedures or tests to generate revenue. There are a number of policies that vary from location to location, but here are some key features of typical value-based care policies:
- Pay-for-performance (P4P): In a value-based care model, healthcare providers are reimbursed based on the quality of care they deliver rather than the volume of services they provide. This means that providers are incentivized to focus on patient outcomes and quality of care rather than the number of procedures or tests they perform.
- Quality metrics: Value-based care policies typically include a set of quality metrics that healthcare providers are measured against. These metrics may include things like patient satisfaction, clinical outcomes and adherence to evidence-based guidelines.
- Care coordination: In a value-based care model, healthcare providers are encouraged to work together to coordinate care for patients. This means that primary care providers, specialists and other healthcare professionals may collaborate to ensure that patients receive the right care at the right time.
- Patient engagement: Value-based care policies prioritize patient engagement, meaning that patients are encouraged to be actively involved in their care. This may involve things like shared decision-making, patient education and support for self-management of chronic conditions.
- Risk sharing: In some value-based care models, healthcare providers may be required to share financial risk with payers, meaning that they may be financially responsible if patients do not achieve good health outcomes. This can incentivize providers to focus on prevention and care coordination to improve patient outcomes.
Value-based care models have the potential to improve healthcare, but there are also challenges that must be addressed. One such challenge is ensuring that risk adjustment is accurate. Risk adjustment is the process of accounting for differences in patient health status and needs when evaluating provider performance. If risk adjustment is not done properly, providers may be unfairly penalized or rewarded for factors outside of their control (e.g. a patient may just have a particularly poor genetic roll of the dice, and be prone to several conditions).
To that end, value-based care models may inadvertently incentivize providers to avoid taking on high-risk patients who are more likely to have poor health outcomes. This can create a cherry picking effect where providers focus on patients who are more likely to respond to interventions and avoid those who are sicker or have more complex needs. This is also a concern as it pertains to insurance companies. If insurers gain access to a patient’s genetic information, it could influence how coverage is applied or priced.
Conclusion
The future of healthcare has never been brighter. Life expectancy is ever increasing, and by many measures quality of life is also increasing. Technological advances have delivered significant improvements in the quality of care people receive, making it more tailored to the individual.
Furthermore, a patient’s access to health information has never been better, allowing individuals to truly participate in driving and understanding their own healthcare-related decisions. However, with the advent of this technology and the data it produces, policies need to keep pace to maintain a focus on the key objective of improving life for humans throughout the world.
About the Author

Travis Schneider is Aerotech’s business development manager for advanced manufacturing market segments, including electronics manufacturing, laser processing, medical technology, data storage and precision manufacturing. He has 13+ years of experience in precision automation and robotics, holding roles in applications engineering, field sales, product management and business development. He has worked alongside several leading medical instrument builders, medical device OEMs, and surgical robotic companies to develop and release products to the market. His expertise and passion for innovation make him an invaluable resource for partners seeking to push boundaries in precision automation for advanced manufacturing.